 Journal of Global Health, 10(1). June 2020
Journal of Global Health, 10(1). June 2020
Basically, their answer is YES.
Only about 20% of patients with COVID-19 develop serious symptoms, which seem to take about a week to come on, giving time to identify those at risk and treat them with antiviral medications.
The authors identified two phases, similar to that of SARS and MERS (also coronavirus illnesses). The first is a “viral” phase in which the viral load increases rapidly, infecting cells and triggering an immune response. The second is the “immune” phase which occurs only in some patients – this is when the immune system loses control, causing serious damage to the lungs, kidneys, and heart — also called a cytokine storm.
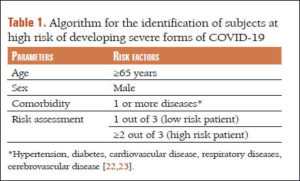
The authors describe their development of an algorithm using data from Italy and China to identify individuals at risk of developing severe or lethal forms of COVID-19. Risk factors are age (65 years or older), male sex, and at least two of the following: hypertension, diabetes, lung disease, heart disease, or brain/blood vessel disease. Using this algorithm, doctors can decide which of their patients are at risk and also which antiviral medications would be suitable based on possible interactions with other medications the patients are taking.
The authors warn that a delay until hospitalization to begin antiviral treatment could reduce its effectiveness, so those at risk should begin treatment at home as early as possible after symptoms or a positive test is observed — and for those at risk, waiting several days for test results could be a problem, so treatment should begin earlier, and then could be stopped if the test results show it is not needed.
The antiviral drugs known to be effective at the time this paper was published (June 2020) were CQ, HCQ, and a combination of Lopinavir and Ritonavir (which would be the preferred treatment for a patient with a prolonged QT (heart abnormality).
Quote: “Early antiviral treatment of symptomatic patients at risk could result in a reduction in the numbers of hospitalizations and intensive care treatments and, therefore, of the related costs incurred by public health systems.